Do you ever find yourself wincing in pain whenever you take a step or put pressure on the top of your foot? It can be quite concerning when you experience foot pain, especially if you’re unsure about its causes. In this article, we will delve into the top seven reasons you might be experiencing discomfort on the top of your foot so you can better understand the underlying issues and find relief.
The seven primary causes of top-of-foot pain are stress fractures, extensor tendonitis, nerve compression, arthritis, and ill-fitting footwear. Each of these factors can contribute to your discomfort, and it’s essential to identify the specific cause to address it effectively. So, if you’ve been curious about what might be causing your foot pain, keep reading as we uncover the details about each condition and how they manifest.
We believe that understanding foot pain in-depth is the first step towards finding lasting relief and maintaining excellent foot health. So, without any further ado, let’s dive into foot pain and discover the insights that will keep you walking comfortably for years.
Understanding Foot Anatomy
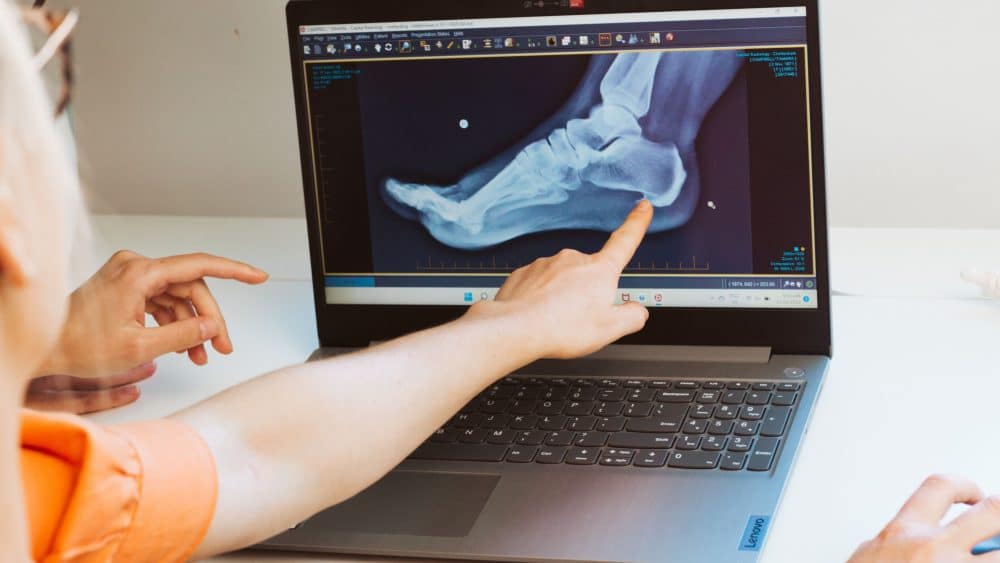
To fully grasp the complexity of foot pain and its causes, it’s crucial to delve into the intricate anatomy of the foot. The human foot is a marvel of engineering, comprising 26 bones, 33 joints, and over 100 muscles, tendons, and ligaments that work in unison to support our body weight and facilitate movement.
- Bones: The foot’s bones are divided into three main sections: the hindfoot, midfoot, and forefoot. The hindfoot includes the talus and calcaneus, commonly known as the heel bone. The midfoot contains five tarsal bones, forming the arch of the foot and providing stability. The forefoot comprises the metatarsal bones, leading to the toes, and the phalanges, which are the toe bones.
- Joints: Joints are the connections between bones that enable movement. The foot’s joints are essential for absorbing shock and maintaining balance. The ankle joint allows the foot to move up and down, while the subtalar joint beneath it allows side-to-side movement.
- Muscles and Tendons: The foot muscles are organised into two groups: the extrinsic muscles, which originate in the lower leg and connect to the foot, and the intrinsic muscles, which are entirely within the foot. These muscles control foot movements, such as pointing and flexing. Tendons are strong, fibrous tissues that connect muscles to bones, transmitting the force produced by the muscles to the bones to move.
- Ligaments: Ligaments are bands of tough, elastic tissue that connect bones, providing stability and preventing excessive movement. The foot’s ligaments are crucial in maintaining the arches and supporting the joints.
- Arches: The foot has three primary arches: the medial longitudinal arch (along the inner side of the foot), the lateral longitudinal arch (along the outer side), and the transverse arch (running across the midfoot). These arches act as shock absorbers, evenly distributing the forces experienced during walking and other activities.
Understanding foot anatomy is fundamental because any disruption or dysfunction within this intricate system can lead to foot pain and discomfort. Conditions such as plantar fasciitis, metatarsalgia, Morton’s neuroma, sesamoiditis, and stress fractures can all arise from various factors affecting the foot’s bones, joints, muscles, and ligaments.
Prioritising foot health and seeking professional advice if experiencing persistent or severe foot pain is essential. A podiatrist or a healthcare practitioner specialising in foot conditions can provide a comprehensive evaluation, accurate diagnosis, and personalised treatment plan to alleviate pain and promote overall foot wellness.
Additionally, maintaining proper foot care, wearing appropriate footwear, and engaging in foot-strengthening exercises can go a long way in preventing and managing foot pain.
Plantar Fasciitis: The Common Culprit
Plantar fasciitis is one of the most prevalent causes of foot pain, and it is estimated that it affects millions of individuals all over the world. This ailment is brought on by an inflammation or irritation of the plantar fascia, which is a thick band of connective tissue that runs along the bottom of the foot from the heel to the toes.
The condition manifests itself when the plantar fascia is inflamed or irritated. Those who engage in strenuous physical activity, notably athletes and those who are required to be on their feet for lengthy periods of time, are more likely to suffer from this condition.
1. Symptoms
- Heel Pain: The hallmark symptom of plantar fasciitis is a pain in the heel, typically felt near the front of the heel bone. The pain can be sharp or dull and may worsen with the first steps in the morning or after prolonged rest periods.
- Arch Pain: In addition to heel pain, some individuals with plantar fasciitis may experience discomfort in the foot’s arch. This pain is due to the inflammation of the plantar fascia, which extends along the length of the foot’s arch.
- Top of Foot Pain: Plantar fasciitis can cause pain on the top of the foot. The inflammation in the plantar fascia can create tension that radiates upwards, leading to discomfort on the foot’s dorsal side.
- Stiffness in the Morning: Many people with plantar fasciitis notice significant stiffness and pain in the foot, particularly in the morning or after extended periods of rest. This is known as post-static dyskinesia and tends to improve with movement throughout the day.
2. Causes
- Overuse or Repetitive Strain: Plantar fasciitis often develops due to repetitive stress on the foot, such as excessive walking, running, or jumping. Athletes who engage in activities that involve repetitive impact on the feet are at a higher risk.
- High-Impact Activities: Activities that subject the foot to high impacts, such as running on hard surfaces or participating in sports like basketball or tennis, can contribute to the development of plantar fasciitis.
- Flat Feet or High Arches: Individuals with flat feet or high arches are more susceptible to plantar fasciitis. Flat feet can cause overstretching of the plantar fascia, while high arches can lead to excessive pressure on the heel and forefoot.
- Improper Footwear: Wearing shoes that lack proper support, particularly those with inadequate arch support or cushioning, can increase the risk of developing plantar fasciitis.
- Tight Calf Muscles: Tightness in the calf muscles can pull on the Achilles tendon, which, in turn, affects the tension on the plantar fascia.
3. Treatment
Fortunately, most cases of plantar fasciitis can be successfully managed with conservative treatments. The following measures can help alleviate pain and promote healing:
- Rest and Avoiding Aggravating Activities: Giving the foot sufficient rest and avoiding activities exacerbating the pain can facilitate healing.
- Stretching Exercises: Gentle stretching exercises for the calf muscles and plantar fascia can help reduce tension and promote flexibility.
- Orthotic Inserts: Custom or over-the-counter orthotic inserts can provide additional support and cushioning, relieving pressure on the plantar fascia.
- Physical Therapy: A physical therapist can recommend specific exercises and techniques to strengthen the foot and ankle and improve overall foot mechanics.
- Ice Therapy: Applying ice to the affected area can help reduce inflammation and alleviate pain.
When conservative treatments do not provide sufficient relief in severe cases, medical interventions such as corticosteroid injections or extracorporeal shock wave therapy may be considered. However, it’s essential to consult a podiatrist for a proper diagnosis and personalised treatment plan to ensure the best outcome.
Taking preventive measures such as wearing appropriate footwear, maintaining a healthy weight, and incorporating regular foot exercises into one’s routine can also significantly reduce the risk of developing plantar fasciitis and promote foot health.
Metatarsalgia: When the Ball of Your Foot Hurts
Metatarsalgia is a painful condition characterised by discomfort in the ball of the foot, the area just behind the toes. This condition can make walking, standing, and other weight-bearing activities challenging and uncomfortable. Metatarsalgia can affect anyone, but it is particularly common among athletes, individuals who engage in high-impact sports, and those who wear improper footwear.
1. Symptoms
- Pain in the Ball of the Foot: The primary symptom of metatarsalgia is pain and tenderness in the ball of the foot. The discomfort may be described as aching, burning, or sharp, and it tends to worsen with activity and improve with rest.
- Pain on the Top of the Foot: In some cases, metatarsalgia can cause pain on the top of the foot. This is often due to the inflammation and irritation of the metatarsal bones and the surrounding tissues.
- Tingling or Numbness: Some individuals with metatarsalgia may experience tingling or numbness in the toes, resulting from pressure on the nerves in the ball of the foot.
2. Causes
- High Heels or Ill-Fitting Footwear: Wearing high heels or shoes with narrow toe boxes can place excessive pressure on the ball of the foot, leading to metatarsalgia. Tight footwear can also cause the toes to become cramped, exacerbating the condition.
- High-Impact Activities: Engaging in activities that involve jumping, running, or abrupt movements can subject the metatarsal bones to repetitive impact, leading to inflammation and pain.
- Foot Deformities: Certain foot deformities, such as hammertoes or bunions, can alter the weight distribution across the foot, increasing the risk of metatarsalgia.
- Age and Foot Structure: As people age, the fat pad in the ball of the foot may thin out, resulting in less natural cushioning. Additionally, individuals with a high arch or a second toe longer than the first (Morton’s toe) are more susceptible to metatarsalgia.
- Weight Distribution: Excessive body weight can strain the metatarsal bones and the surrounding tissues, contributing to foot pain.
3. Treatment
The treatment for metatarsalgia focuses on reducing pain, addressing the underlying causes, and preventing future occurrences. Some effective treatment options include:
- Wearing Comfortable and Supportive Footwear: Choosing shoes with ample cushioning, a wide toe box, and good arch support can help alleviate pressure on the ball of the foot and promote proper weight distribution.
- Using Metatarsal Pads: Metatarsal pads or orthotic inserts can be placed in the shoes to provide extra support to the metatarsal area and relieve pressure.
- Rest and Ice Therapy: Giving the foot adequate rest and applying ice to the affected area can help reduce inflammation and pain.
- Physical Therapy: A physical therapist can recommend exercises to strengthen the foot muscles and improve flexibility, aiding recovery.
In severe or persistent cases, a healthcare practitioner may recommend corticosteroid injections to reduce inflammation or suggest surgical intervention for foot deformities contributing to metatarsalgia.
Preventing metatarsalgia involves being mindful of footwear choices, avoiding high heels for extended periods, and maintaining healthy body weight. Additionally, warming up before exercise, engaging in low-impact activities, and performing foot-strengthening exercises can help reduce the risk of developing metatarsalgia and maintain foot health.
As with any foot condition, seeking medical advice for an accurate diagnosis and personalised treatment plan is essential to ensure the best outcome and relieve foot pain effectively.
Morton’s Neuroma: Nerve Pain in the Toes
Morton’s Neuroma is a painful condition that involves the thickening of the tissue around one of the nerves leading to the toes, most commonly between the third and fourth toes. This enlargement of the nerve can cause significant discomfort and lead to sensations of burning, tingling, or numbness in the toes. Morton’s Neuroma can affect people of all ages and activity levels, but it is more prevalent in women and individuals who wear tight, narrow, or high-heeled shoes.
1. Symptoms
- Sharp, Burning Pain: The primary symptom of Morton’s Neuroma is a sharp, burning pain in the ball of the foot, particularly between the affected toes. The pain may radiate into the toes or back toward the foot’s arch.
- Numbness or Tingling: Individuals with Morton’s Neuroma often experience sensations of tingling or numbness in the toes, which can be triggered or exacerbated by pressure on the foot.
2. Causes
- Compression or Irritation of the Nerve: Morton’s Neuroma occurs when the nerve between the toes becomes compressed or irritated, leading to inflammation and the development of a thickened mass of tissue around the nerve.
- Improper Footwear: Wearing shoes with a narrow toe box or high heels can squeeze the toes together, increasing pressure on the nerve and contributing to the development of Morton’s Neuroma.
- Foot Deformities: Certain foot deformities, such as bunions, hammertoes, or flat feet, can alter the foot’s structure and increase the risk of nerve compression.
- Repetitive Stress: Engaging in activities that involve repetitive stress on the forefoot, such as running or high-impact sports, can also contribute to the development of Morton’s Neuroma.
3. Treatment
The treatment for Morton’s Neuroma aims to relieve pain, reduce inflammation, and prevent further irritation of the affected nerve. Several conservative treatment options can effectively manage the condition, including:
- Wearing Shoes with a Wide Toe Box: Choosing footwear that provides ample room for the toes and reduces pressure on the affected nerve can significantly improve symptoms.
- Using Metatarsal Pads: Metatarsal pads or orthotic inserts placed in the shoes can help spread the metatarsal bones and alleviate pressure on the nerve.
- Corticosteroid Injections: In cases where the pain is severe, corticosteroid injections may be administered to reduce inflammation and relieve discomfort.
- Modifying Activities: Avoiding high-impact activities and exercises that worsen symptoms can allow the inflamed nerve to heal.
- Applying Ice: Ice to the affected area can help reduce inflammation and relieve temporary pain.
- Footwear Modifications: A podiatrist may recommend custom orthotics or footwear modifications to provide better support and alleviate pressure on the affected nerve.
In cases where conservative treatments fail to provide relief, more invasive measures, such as alcohol sclerosing injections or surgical removal of the affected nerve, may be considered.
Preventing Morton’s Neuroma involves wearing appropriate footwear that allows the toes to move freely and maintaining a healthy weight to reduce pressure on the forefoot. Additionally, avoiding activities that place excessive stress on the feet can help reduce the risk of developing this painful condition.
Sesamoiditis: Pain under the Big Toe
Sesamoiditis is a painful condition characterised by inflammation of the sesamoid bones, two small, pea-shaped bones beneath the big toe joint in the foot. These tiny bones act as pulleys for the tendons, allowing smooth movement of the big toe and providing stability to the foot during activities like walking, running, and jumping. When these bones become inflamed or irritated, it can lead to significant pain and discomfort, particularly under the big toe.
1. Symptoms
- Pain under the Big Toe: The primary symptom of sesamoiditis is pain localised under the big toe joint. The pain may be sharp, throbbing, or achy and worsens with weight-bearing activities.
- Pain on the Top of the Foot: In some cases, sesamoiditis can cause pain on the top of the foot, as the sesamoid bones are close to the skin’s surface.
- Swelling and Bruising: Inflammation of the sesamoid bones can lead to swelling and bruising in the affected area.
2. Causes
- Overuse or Repetitive Pressure: Sesamoiditis often develops due to overuse or excessive pressure on the sesamoid bones. Activities that involve repeated bending of the big toe, such as dancing or running, can contribute to the condition.
- High Heels or Tight Footwear: Wearing high heels or shoes with a narrow toe box can increase pressure on the sesamoid bones, leading to inflammation.
- Foot Structure: Individuals with a high arch or prominent or elongated first metatarsal bone may be more susceptible to sesamoiditis.
- Foot Trauma: Direct trauma or impact to the ball of the foot can result in sesamoiditis.
3. Treatment
The treatment for sesamoiditis focuses on relieving pain, reducing inflammation, and allowing the sesamoid bones to heal. Several conservative treatment options can effectively manage the condition, including:
- Rest and Activity Modification: Resting the foot and avoiding activities exacerbating the pain can promote healing.
- Icing: Applying ice to the affected area can help reduce inflammation and alleviate pain.
- Pain Relief Medications: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) can manage pain and reduce inflammation.
- Padding and Taping: Padding the ball of the foot or taping the big toe can support and reduce pressure on the sesamoid bones.
- Orthotic Inserts: Custom orthotic inserts or metatarsal pads can offload pressure from the sesamoid bones and support the foot arch.
- Changes in Footwear: Wearing shoes with a wide toe box and adequate cushioning can help reduce pressure on the sesamoid bones.
Stress Fractures: Tiny Cracks with Significant Pain
Stress fractures are small cracks in the bones, commonly occurring in weight-bearing bones, that result from repetitive and excessive stress on the bone. Unlike acute fractures caused by a sudden impact or trauma, stress fractures develop over time due to the cumulative effect of repetitive activities. These fractures can be particularly problematic in the foot, where the bones endure significant pressure during daily activities like walking, running, and jumping.
1. Symptoms
- Pain During Weight-Bearing Activities: The hallmark symptom of a stress fracture is pain that intensifies during weight-bearing activities, such as walking or running. The pain often decreases with rest.
- Swelling and Tenderness: The affected area may become swollen and tender to the touch. Pressing on the bone may elicit increased discomfort.
- Pain That Improves with Rest: Stress fractures tend to worsen with activity and improve with rest. However, as the condition progresses, the pain may become persistent and be present even during periods of rest.
2. Causes
- Overuse or Repetitive Stress: Engaging in activities that involve repetitive impact on the foot, such as running, dancing, or jumping, can lead to stress fractures. Athletes and individuals who suddenly increase their exercise intensity are at a higher risk.
- Weakened Bones: Bones can become weakened due to conditions such as osteoporosis or nutritional deficiencies, making them more susceptible to stress fractures.
- Sudden Increase in Physical Activity: Abruptly increasing the intensity, duration, or frequency of physical activity can overwhelm the bones’ ability to repair and adapt, leading to stress fractures.
3. Treatment
The treatment for stress fractures aims to promote bone healing and prevent further damage. Common approaches include:
- Immobilisation with a Cast or Boot: In severe cases, the foot may need to be immobilised with a cast or walking boot to allow the bone to heal properly.
- Rest and Avoidance of High-Impact Activities: Rest is crucial for healing the bone. Avoiding activities that stress the affected foot can help prevent further damage.
- Gradual Return to Activities: Once the fracture has healed, a gradual return to weight-bearing activities under the guidance of a healthcare practitioner or physical therapist can help prevent re-injury.
- Pain Relief Medications: Over-the-counter pain relievers may be recommended to manage discomfort and inflammation.
- Nutritional Supplements: In cases where nutritional deficiencies contribute to weakened bones, supplements may be prescribed to support bone health.
4. Prevention
Preventing stress fractures involves taking measures to reduce the risk of bone overuse and weakness:
- Proper Footwear: Wearing appropriate footwear with sufficient cushioning and support can help absorb shock and reduce bone stress.
- Gradual Training Progression: Gradually increasing the intensity and duration of exercise can allow the bones to adapt and strengthen over time.
- Cross-Training: Incorporating low-impact activities like swimming or cycling into the exercise routine can help reduce bone strain.
- Adequate Nutrition: A balanced diet rich in calcium, vitamin D, and other essential nutrients can support bone health.
Stress fractures require prompt medical attention to ensure proper healing and prevent complications. If an individual suspects a stress fracture, it is essential to consult a podiatrist for an accurate diagnosis and personalised treatment plan. Following the prescribed treatment and preventive measures can aid in a speedy recovery and reduce the risk of future stress fractures.
Midfoot Arthritis
Midfoot arthritis is a condition that mostly impacts the central region of the foot, mainly targeting joints such as the tarsometatarsal and naviculocuneiform joints. This particular kind of arthritis is characterised by its notable influence on the quality of life for individuals affected, necessitating a cautious and nuanced approach to therapeutic interventions.
The midfoot region is pivotal in the biomechanics of ambulation and locomotion, enduring significant magnitudes of force with every stride. The occurrence of uncomfortable closeness between the joints can be attributed to several sources, including prolonged pressure exerted on the midfoot joints. This condition can significantly impede individuals’ ability to carry out their everyday tasks.
1. Symptoms
Midfoot arthritis is frequently characterised by discomfort experienced in the plantar region of the foot, particularly during ambulation or weight-bearing activities. Furthermore, it is common for individuals to have other symptoms, which may include:
- Individuals may experience discomfort when wearing shoes that lack flexibility, especially when there is pressure exerted on the dorsal aspect of the foot.
- First-step discomfort.
- The presence of edema in the region encompassing the midfoot.
- The individual has heightened discomfort while encountering uneven terrain or engaging in stair-related activities.
- Foot instability.
In the absence of appropriate management, midfoot arthritis can induce midfoot collapse, hence giving rise to a stiff flatfoot deformity accompanied by the formation of bony spurs. This problem can cause significant discomfort and pose difficulties in finding footwear that is both suitable in size and provides comfort.
2. Causes
Midfoot arthritis is predominantly attributed to progressive degeneration; however, it may be classified into five distinct etiological factors:
- Post-traumatic: This refers to the development of arthritis in the midfoot region subsequent to an accident, such as fractures or Lisfranc injuries.
- Inflammatory: Chronic inflammation resulting from ailments such as rheumatoid arthritis can do significant harm to the joints, ultimately resulting in the development of midfoot arthritis, which frequently affects many joints simultaneously.
- Neuropathic: This is frequently encountered in cases of Charcot foot and is characterised by arthritis resulting from neuropathy.
- Post hindfoot fusion: Hindfoot fusion is a surgical procedure that involves the union of bones in the rearfoot. However, it has been seen that midfoot arthritis might develop as a consequence of this treatment.
- Degenerative: The gradual deterioration of cartilage and joints over a period of time as a result of mechanical stress and strain.
The significance of footwear quality is particularly evident in its impact on degenerative damage. Choosing footwear that provides enough support and midfoot stiffness is crucial, given that the midfoot region naturally exhibits restricted flexibility. Certain footwear with inadequate support might lead to abnormal bending, resulting in elevated midfoot compressive stresses and degenerative conditions.
3. Treatment
1. Foot or Joint Mobilisation Therapy
Foot Mobilisation Techniques (FMT) refer to a manual treatment approach that aims to optimise the functionality of the foot and ankle. This study focuses on examining stiffness, misalignment, and dysfunction within the aforementioned joints. Foot and ankle mobilisation and manipulation techniques (FMT) are utilised to improve the functionality of the lower limb.
These targeted motions are employed to enhance the function of the foot, ankle, and lower limb. The objective is to attain a state of joint mobility without discomfort by utilising delicate manual methods, in conjunction with stretching and strengthening exercises, to maximise desired results.
The utilisation of foot mobilisation has been found to provide positive outcomes in a number of scenarios, including instances where individuals have musculoskeletal discomfort, biomechanical compensations, or limitations in joint range of motion.
The technique is notably efficient in alleviating connective tissue constraints, enhancing foot mobility and yielding improved outcomes when used with orthotic therapy.
2. Surgical Treatment
In cases where non-surgical interventions fail to mitigate the handicap caused by persistent pain, fusion surgery may be deemed required. The aforementioned method entails the extraction of impaired cartilage and the establishment of enduring joint stabilisation. The conventional approach involves using plates, screws, or wires to immobilise the joint.
Dorsal Midfoot Impingement
This particular ailment results in persistent and substantial discomfort experienced on the weight-bearing area of the foot’s upper side (dorsal aspect) during physical activities.
The occurrence of discomfort results from recurrent stress exerted on the surface of the dorsal mid-foot joints, leading to inflammation inside the ligaments. Wearing shoes with minimal or no heel elevation may exacerbate discomfort, whilst opting for shoes with a slightly higher heel may reduce symptoms.
Individuals who engage in forefoot striking and utilise minimalist footwear may potentially experience a higher vulnerability to “top of foot pain” due to amplified dorsiflexion motions involving the forefoot and rearfoot.
1. Symptoms
The clinical presentation of dorsal midfoot impingement commonly includes bilateral foot pain and discomfort at the dorsal joint. Furthermore, there may be other symptoms that can be observed:
- The individual experiences discomfort localised in the heel and arch regions.
- The sensation of pain experienced in the morning.
- The level of discomfort and agony experienced progressively intensifies.
- The presence of sensory abnormalities such as numbness, tingling, and burning feelings in the foot.
- The existence of a protuberance located on the dorsal aspect of the foot.
2. Causes
The application of excessive force on the articulations located in the upper region of the midfoot has the potential to initiate the structural failure of the arch of the foot. This action results in the extension of the arch and the reduction in length of the upper part of the foot, leading to the generation of pressure inside the bones.
The occurrence of midfoot collapse can be influenced by many circumstances, such as:
- Weight-bearing activities which refer to physical exercises or movements that require an individual to support their body weight through their bones and muscles.
- Restricted range of motion in the ankle joint.
- The process of increasing one’s bodily weight.
- Repetitive stress refers to the physiological strain experienced by individuals due to the repeated performance of certain activities or movements.
- Inadequately sized footwear.
- The individual presents with a condition characterised by a taut Achilles tendon.
- Tightened gastrocnemius muscles.
- Arthritis might result from prior instances of fracture, surgical procedures, or traumatic events.
- Biomechanical anomalies, such as excessive arches or reduced arches in the foot.
3. Treatment
1. Foot or Joint Mobilisation Therapy
Like with midfoot arthritis, we can treat dorsal midfoot impingement by foot or joint mobilisation therapy. Foot Mobilisation Techniques (FMT) refer to a manual therapeutic strategy to enhance the functionality of the foot and ankle. This approach specifically addresses stiffness, misalignment, and dysfunction within these joints.
The primary objective of foot and ankle mobilisation and manipulation techniques is to optimise the functioning of the lower limb. The actions above are employed with the aim of enhancing the performance of the foot, ankle, and lower limb. To produce the most favourable outcomes, the objective is to get joint mobility without discomfort by employing mild manual methods in conjunction with stretching and strengthening exercises.
This intervention has demonstrated significant efficacy in the alleviation of connective tissue limitations, leading to improved mobility of the foot and enhanced treatment results when utilised in conjunction with orthotic therapy.
2. Other Treatment Options
When detected at an early stage, dorsal midfoot impingement often exhibits favourable responses to non-surgical therapies. The available treatment options encompass:
- Supportive footwear (shoes designed to provide assistance and stability to the feet, particularly during physical activities).
- The use of orthotic devices as a preventive measure against arch collapse.
- Modifications to physical activity, recreational pursuits, or daily regimen.
- Exercise therapy (a treatment approach that utilises physical activity to improve and restore physical function).
- Low-level laser therapy (LLLT) is a therapeutic modality that utilises low-power lasers or light-emitting diodes (LEDs) to stimulate cellular function.
In order to effectively manage injuries, it is imperative to identify and address any underlying mechanical issues under the supervision of a qualified podiatrist. Therefore, it is imperative to evaluate biomechanics and gait before initiating therapy.
Conclusion
In conclusion, understanding the causes of top-of-foot pain is crucial in maintaining overall foot health and ensuring a pain-free lifestyle. Throughout this blog, we have explored seven common reasons behind this discomfort and gained valuable insights into potential remedies. Remember, proper foot care and regular visits to a podiatrist can make a significant difference in alleviating or preventing such pain.
Now that you know the common causes of top-of-foot pain, which of these factors resonates the most with your experiences? Is there a particular cause you have faced in the past, and if so, how did you find relief? Share your thoughts and stories in the comments below, and let’s help each other on our journey to healthier and happier feet!
Content Summary
- To fully grasp the complexity of foot pain and its causes, it’s crucial to delve into the intricate anatomy of the foot.
- The foot’s ligaments are crucial in maintaining the arches and supporting the joints.
- Conditions such as plantar fasciitis, metatarsalgia, Morton’s neuroma, sesamoiditis, and stress fractures can all arise from various factors affecting the foot’s bones, joints, muscles, and ligaments.
- Prioritising foot health and seeking professional advice if experiencing persistent or severe foot pain is essential.
- Additionally, maintaining proper foot care, wearing appropriate footwear, and engaging in foot-strengthening exercises can go a long way in preventing and managing foot pain.
- Plantar fasciitis is one of the most prevalent causes of foot pain, and it is estimated that it affects millions of individuals all over the world.
- In addition to heel pain, some individuals with plantar fasciitis may experience discomfort in the foot’s arch.
- Plantar fasciitis can cause pain on the top of the foot.
- Many people with plantar fasciitis notice significant stiffness and pain in the foot, particularly in the morning or after extended periods of rest.
- Plantar fasciitis often develops due to repetitive stress on the foot, such as excessive walking, running, or jumping.
- Athletes who engage in activities that involve repetitive impact on the feet are at a higher risk.
- A physical therapist can recommend specific exercises and techniques to strengthen the foot and ankle and improve overall foot mechanics.
- Applying ice to the affected area can help reduce inflammation and alleviate pain.
- However, it’s essential to consult a podiatrist for a proper diagnosis and personalised treatment plan to ensure the best outcome.
- Preventive measures such as wearing appropriate footwear, maintaining a healthy weight, and incorporating regular foot exercises into one’s routine can also significantly reduce the risk of developing plantar fasciitis and promote foot health.
- Metatarsalgia is a painful condition characterised by discomfort in the ball of the foot, the area just behind the toes.
- The primary symptom of metatarsalgia is pain and tenderness in the ball of the foot.
- Metatarsalgia can sometimes cause pain on the top of the foot.
- Additionally, individuals with a high arch or a second toe longer than the first (Morton’s toe) are more susceptible to metatarsalgia.
- The treatment for metatarsalgia focuses on reducing pain, addressing the underlying causes, and preventing future occurrences.
- Choosing shoes with ample cushioning, a wide toe box, and good arch support can help alleviate pressure on the ball of the foot and promote proper weight distribution.
- Preventing metatarsalgia involves being mindful of footwear choices, avoiding high heels for extended periods, and maintaining healthy body weight.
- As with any foot condition, seeking medical advice for an accurate diagnosis and personalised treatment plan is essential to ensure the best outcome and relieve foot pain effectively.
- Morton’s Neuroma is a painful condition that involves the thickening of the tissue around one of the nerves leading to the toes, most commonly between the third and fourth toes.
- Individuals with Morton’s Neuroma often experience sensations of tingling or numbness in the toes, which can be triggered or exacerbated by pressure on the foot.
- The treatment for Morton’s Neuroma aims to relieve pain, reduce inflammation, and prevent further irritation of the affected nerve.
- Choosing footwear that provides ample room for the toes and reduces pressure on the affected nerve can significantly improve symptoms.
- In cases where conservative treatments fail to provide relief, more invasive measures, such as alcohol sclerosing injections or surgical removal of the affected nerve, may be considered.
- Sesamoiditis is a painful condition characterised by inflammation of the sesamoid bones, two small, pea-shaped bones beneath the big toe joint in the foot.
- When these bones become inflamed or irritated, it can lead to significant pain and discomfort, particularly under the big toe.
- The primary symptom of sesamoiditis is pain localised under the big toe joint.
- In some cases, sesamoiditis can cause pain on the top of the foot, as the sesamoid bones are close to the skin’s surface.
- The treatment for sesamoiditis focuses on relieving pain, reducing inflammation, and allowing the sesamoid bones to heal.
- Resting the foot and avoiding activities exacerbating the pain can promote healing.
- Stress fractures are small cracks in the bones, commonly occurring in weight-bearing bones, that result from repetitive and excessive stress on the bone.
- Unlike acute fractures caused by a sudden impact or trauma, stress fractures develop over time due to the cumulative effect of repetitive activities.
- The hallmark symptom of a stress fracture is pain that intensifies during weight-bearing activities, such as walking or running.
- Engaging in activities that involve repetitive impact on the foot, such as running, dancing, or jumping, can lead to stress fractures.
- The treatment for stress fractures aims to promote bone healing and prevent further damage.
- Stress fractures require prompt medical attention to ensure proper healing and prevent complications.
- If an individual suspects a stress fracture, it is essential to consult a healthcare practitioner for an accurate diagnosis and personalised treatment plan.
- Following the prescribed treatment and preventive measures can aid in a speedy recovery and reduce the risk of future stress fractures.
- In conclusion, understanding the causes of top-of-foot pain is crucial in maintaining overall foot health and ensuring a pain-free lifestyle.
- Throughout this blog, we have explored seven common reasons behind this discomfort and gained valuable insights into potential remedies.
- Remember, proper foot care and regular visits to a podiatrist can make a significant difference in alleviating or preventing such pain.
FAQs
1. Can I treat plantar fasciitis at home?
Yes, mild cases of plantar fasciitis can often be managed at home with rest, ice, and stretching exercises. However, severe or chronic cases may require medical intervention.
2. Are there any exercises to prevent metatarsalgia?
Yes, exercises that strengthen the foot muscles and improve flexibility can help reduce the risk of developing metatarsalgia.
3. Can Morton’s neuroma be cured without surgery?
In many cases, non-surgical treatments like wearing proper footwear and using orthotic devices can alleviate the symptoms of Morton’s neuroma.
4. Is sesamoiditis more common in athletes?
Sesamoiditis is more common in individuals who participate in activities that involve repetitive pressure on the ball of the foot, such as running and dancing.
5. How long does it take for a stress fracture to heal?
The healing time for a stress fracture varies depending on the location and severity of the fracture but can range from several weeks to a few months.